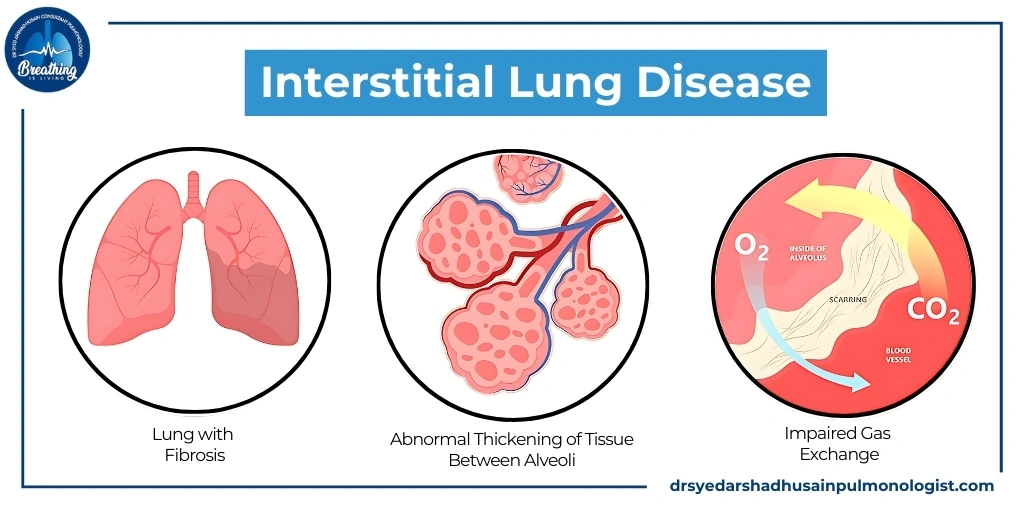
Interstitial lung diseases are a very severe type of condition which causes progressive scarring of lung tissue, which can create breathing problems and reduce oxygen levels in the blood. That�s why it is important to understand this condition as soon as you can so that you can get the appropriate treatment at the right time.
What is Interstitial Lung Disease?
Interstitial lung disease refers to a broad category of lung disorders characterized by inflammation and scarring (fibrosis) of the lung�s interstitium�the tissue and space around the air sacs of the lungs. This scarring thickens the lung tissue, making it difficult for oxygen to pass into the bloodstream, leading to breathing problems and other health issues.
Types of Interstitial Lung Disease
- Idiopathic Pulmonary Fibrosis (IPF): A chronic, progressive lung disease with unknown cause.
- Sarcoidosis: An inflammatory disease causing granulomas in various organs, including lungs.
- Hypersensitivity Pneumonitis: Immune system response to inhaled organic dusts, leading to lung inflammation.
- Connective Tissue Disease-Related ILD: Lung inflammation associated with autoimmune connective tissue diseases.
- Pneumoconiosis: Lung disease caused by inhaling inorganic dust, such as asbestos or silica.
- Cryptogenic Organizing Pneumonia (COP): A rare ILD with inflammation and scarring of small airways and alveoli.
- Nonspecific Interstitial Pneumonia (NSIP): A lung disease with inflammation and scarring, often related to autoimmune disorders.
- Acute Interstitial Pneumonia (AIP): A rare, rapidly progressing ILD causing widespread lung damage.
- Radiation-Induced ILD: Lung damage resulting from radiation therapy, typically used in cancer treatment.
- Drug-Induced ILD: Lung inflammation and scarring caused by certain medications or drug therapies.
Causes of Interstitial Lung Disease
- Occupational and Environmental Exposure: Inhalation of harmful substances like asbestos, silica, or coal dust.
- Autoimmune Diseases: Conditions like rheumatoid arthritis or lupus causing inflammation and lung damage.
- Genetic Factors: Inherited mutations increasing susceptibility to interstitial lung disease in families.
- Medications and Treatments: Certain drugs and radiation therapy leading to lung inflammation and scarring.
- Infections: Viral, bacterial, or fungal infections that cause chronic lung inflammation and fibrosis.
Symptoms of Interstitial Lung Disease
The symptoms of ILD can vary depending on the specific type and the extent of lung damage. However, common symptoms include:
1. Shortness of Breath:
- Description: Difficulty breathing, especially during physical activity, is often the first noticeable symptom of ILD. As the disease progresses, shortness of breath can occur even at rest.
2. Chronic Dry Cough:
- Description: A persistent dry cough that doesn�t produce mucus and doesn�t go away with standard cough remedies is a hallmark of ILD.
3. Fatigue and Weakness:
- Description: ILD can cause a general feeling of tiredness and weakness, making it difficult to carry out daily activities.
4. Chest Pain or Discomfort:
- Description: Some individuals may experience discomfort or a feeling of tightness in the chest.
5. Clubbing of Fingers:
- Description: The tips of the fingers may become enlarged and rounded, a condition known as �clubbing,� often associated with chronic lung diseases.
6. Unintentional Weight Loss:
- Description: Rapid weight loss without a clear reason can occur, often as the disease progresses
Diagnosis of Interstitial Lung Disease
Diagnosing ILD involves a combination of clinical evaluation, imaging tests, and sometimes lung biopsies.
1. Physical Examination:
- Auscultation: A doctor may listen to the lungs with a stethoscope for abnormal sounds, such as crackles, which may indicate ILD.
2. Imaging Tests:
- Chest X-Ray: Can reveal patterns of lung scarring or other abnormalities.
- High-Resolution CT Scan: Provides detailed images of the lungs, helping to identify the extent and pattern of scarring.
3. Pulmonary Function Tests (PFTs):
- Spirometry: Measures how much air you can breathe in and out, and how quickly you can do it.
- Diffusing Capacity Test: Assesses how well oxygen passes from the lungs into the blood.
4. Lung Biopsy:
- Surgical Procedure: In some cases, a small sample of lung tissue is removed and examined under a microscope to determine the specific type of ILD.
Treatment of Interstitial Lung Disease
While there is no cure for ILD, treatment focuses on managing symptoms, slowing disease progression, and improving quality of life.
1. Medications:
- Anti-Inflammatory Drugs: Corticosteroids are often prescribed to reduce lung inflammation.
- Antifibrotic Agents: Drugs like pirfenidone and nintedanib can help slow the progression of fibrosis in some forms of ILD, such as IPF.
- Immunosuppressants: These medications help reduce the immune system�s attack on lung tissue in autoimmune-related ILD.
2. Oxygen Therapy:
- Usage: Supplemental oxygen may be required to maintain adequate oxygen levels in the blood, especially during exercise or sleep.
3. Pulmonary Rehabilitation:
- Programs: Structured exercise and education programs designed to improve lung function, reduce symptoms, and enhance overall well-being.
4. Lifestyle Changes:
- Smoking Cessation: If you smoke, quitting is the most critical step in managing ILD.
- Healthy Diet: A balanced diet rich in nutrients can help maintain energy levels and overall health.
Prevention of Interstitial Lung Disease
While not all types of ILD can be prevented, certain measures can reduce the risk of developing the condition or slow its progression.
1. Avoiding Environmental Hazards:
- Workplace Safety: Protect yourself from inhaling harmful dust, chemicals, and fumes by using protective equipment and following safety guidelines.
- Home Environment: Ensure your home is free from asbestos, mold, and other airborne irritants.
2. Regular Health Checkups:
- Monitoring: Regular checkups can help detect early signs of lung problems, especially if you are at higher risk due to occupational exposure or family history.
3. Vaccinations:
- Influenza and Pneumonia Vaccines: Keeping up with vaccinations can prevent respiratory infections that might exacerbate ILD.
4. Managing Chronic Conditions:
- Autoimmune Disorders: Proper management of autoimmune diseases like rheumatoid arthritis can reduce the risk of associated ILD.
Conclusion
Interstitial lung disease is a very serious disease that requires careful management and a proactive approach. Understanding the symptoms of interstitial lung disease, seeking early diagnosis, and adhering to a comprehensive treatment plan are essential steps in managing ILD. If you want to get relief from interstitial lung diseases, then you should consider an expert such as Prof. Dr. Syed Arshad Husain, known as the best pulmonologist in Dubai.